TENS Treatment for Osteoarthritis: A Comprehensive Guide to Pain Management
Osteoarthritis (OA) is a degenerative joint disease affecting millions worldwide, characterized by the breakdown of cartilage, leading to pain, stiffness, and reduced joint function. While there’s no cure for OA, various treatments aim to manage symptoms and improve quality of life. Transcutaneous Electrical Nerve Stimulation (TENS) is a non-invasive, drug-free option gaining traction as an adjunctive therapy for OA pain. This detailed article explores TENS treatment for osteoarthritis, covering its indications, optimal electrode placement, mechanism of action, frequency, duration, expected results, and potential side effects.
What is TENS?
TENS involves a small, battery-powered device that delivers low-voltage electrical currents through electrodes placed on the skin. These electrical impulses stimulate nerves, aiming to interrupt pain signals or trigger the body’s natural pain-relieving mechanisms.
Indications for TENS in Osteoarthritis
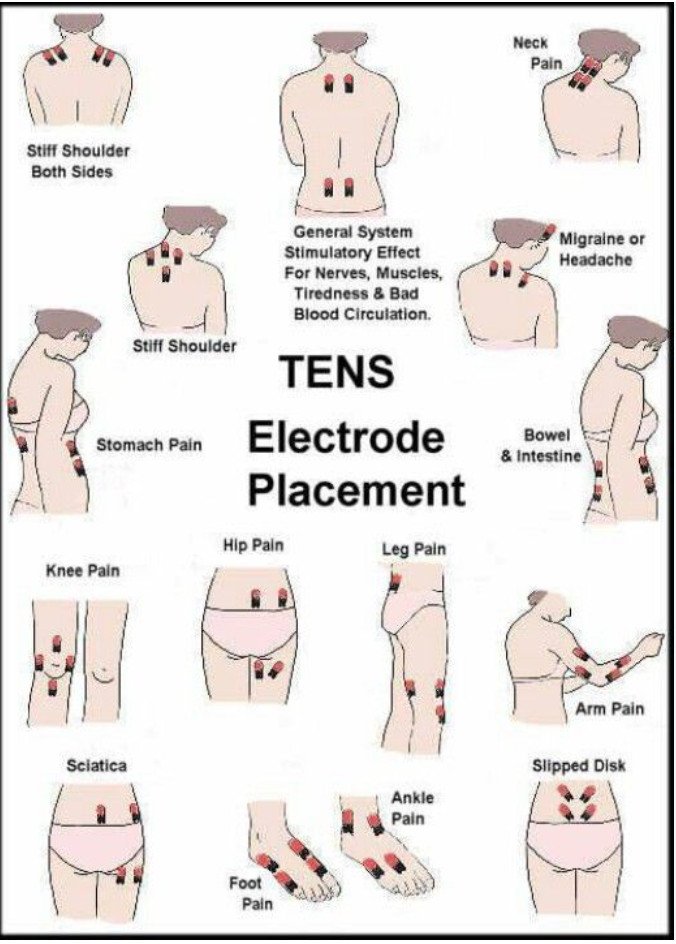
TENS is typically indicated for individuals experiencing pain associated with osteoarthritis, particularly when other conservative measures like medication, exercise, or physical therapy haven’t provided sufficient relief, or when a non-pharmacological option is preferred. It can be used for OA affecting various joints, including:
- Knees: The most common site for OA and TENS application.
- Hips: While more challenging for electrode placement, TENS can be beneficial.
- Hands (fingers, wrist): Particularly useful for managing pain and stiffness in smaller joints.
- Shoulders: For glenohumeral or acromioclavicular joint OA.
- Spine (neck and lower back): For spinal osteoarthritis causing localized pain.
TENS is often considered a supportive therapy and should be integrated into a broader management plan for OA.
Site of Electrode Applications for Osteoarthritis
Precise electrode placement is crucial for maximizing TENS effectiveness in OA. The general principle is to position electrodes directly over or around the painful joint. Here are specific guidelines for common OA sites:
- Knee Osteoarthritis:
- Directly around the joint: Place one electrode on each side of the kneecap (patella), or one above and one below the kneecap.
- Targeting pain points: If pain is localized to a specific area (e.g., medial side of the knee), place electrodes on either side of that painful spot.
- Criss-cross pattern: For widespread knee pain, a criss-cross pattern (one electrode above and to the outside, and one below and to the inside; then repeat on the other side) can be effective.
- Hand/Finger Osteoarthritis:
- Small joints: Place electrodes on either side of the affected joint, or one above and one below. Smaller, specialized electrodes are often available for these areas.
- Wrist: Place electrodes on the dorsal and palmar aspects of the wrist, or on either side of the joint.
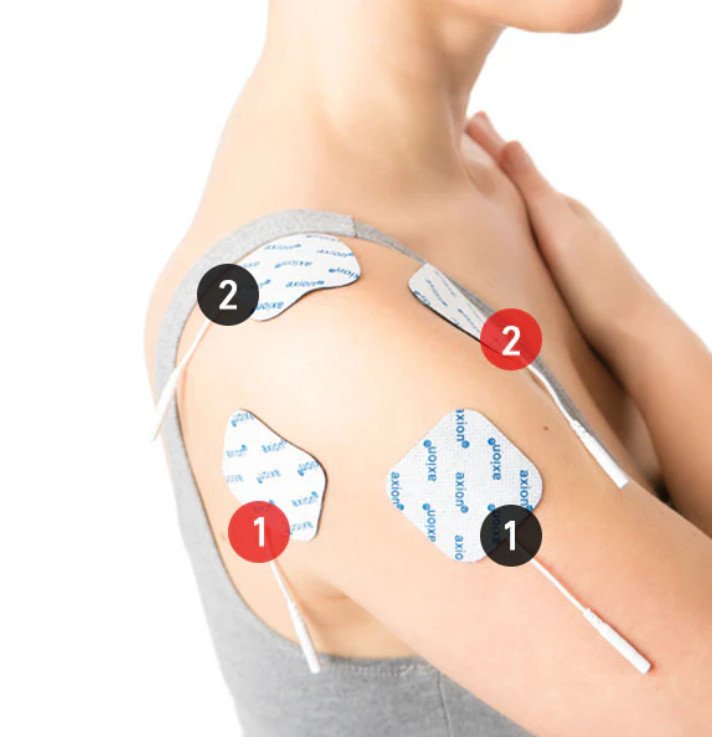
- Shoulder Osteoarthritis:
- Around the joint: Place electrodes around the shoulder joint, targeting the areas of most significant pain (e.g., anterior, posterior, superior aspects).
- Muscle bellies: If muscle spasms accompany the joint pain, electrodes can be placed over relevant muscle bellies (e.g., deltoid, supraspinatus).
- Hip Osteoarthritis:
- Challenges: Hip joint pain can be deep-seated, making precise electrode placement challenging.
- Approaches: Electrodes can be placed over the greater trochanter (bony prominence on the side of the hip) and anteriorly in the groin area. Alternatively, place them on either side of the most palpable painful area in the hip region. Deeper penetration may require higher intensity settings.
- Spinal Osteoarthritis (Neck/Lower Back):
- Refer to general back pain guidelines: Similar to TENS for general back pain, electrodes are placed on either side of the spine at the level of pain, or surrounding the painful area. Avoid placing directly over the spinal column.
Important considerations for electrode placement:
- Clean and dry skin: Always ensure the skin is clean, dry, and free of lotions or oils to ensure optimal adhesion and electrical conduction.
- Avoid sensitive areas: Never place electrodes over open wounds, rashes, infected skin, or areas of numbness.
- Maintain separation: Electrodes should be at least one inch apart and should not touch each other.
- Experimentation: Finding the optimal placement often requires some experimentation, as individual pain patterns vary.
- Refer to instructions: Always follow the specific instructions provided with your TENS unit and consult a healthcare professional or physical therapist for personalized guidance.
Mechanism of Action
The pain-relieving mechanisms of TENS are thought to involve two primary theories, similar to its use for back pain:
- Gate Control Theory: This is the most widely accepted theory. TENS delivers non-painful electrical impulses that stimulate large-diameter, fast-conducting nerve fibers (A-beta fibers). These A-beta fibers “close a gate” in the spinal cord, preventing pain signals from smaller, slow-conducting pain fibers (C-fibers and A-delta fibers) from reaching the brain. This effectively reduces the perception of pain by overriding the pain signals. This mechanism is primarily associated with high-frequency TENS.
- Endorphin Release: TENS, particularly at lower frequencies and higher intensities, can stimulate the release of endogenous opioids, such as endorphins and enkephalins, from the brain and spinal cord. These natural pain-relieving chemicals bind to opioid receptors, leading to an analgesic effect. This mechanism often results in a longer-lasting pain relief after the TENS unit is turned off.
For osteoarthritis, TENS is believed to alleviate pain by both directly interfering with pain signals and by promoting the body’s natural pain-modulating systems. It does not directly treat the joint degeneration itself but offers symptomatic relief.
Frequency and Duration of Treatment
TENS units offer adjustable parameters that can be tailored to individual needs and the type of pain.
- Frequency (Hz):
- High-frequency TENS (Conventional TENS): Typically 80-120 Hz, with a narrow pulse width (e.g., 50-100 µs). This setting produces a comfortable tingling sensation without muscle contraction. It’s often used for immediate pain relief and is thought to primarily engage the gate control theory. It can be used for longer periods.
- Low-frequency TENS (Acupuncture-like TENS): Typically 1-10 Hz, with a wider pulse width (e.g., 150-250 µs). This setting aims to produce visible muscle twitching or contraction. It’s believed to stimulate endorphin release and may offer longer-lasting pain relief. Due to muscle contraction, it’s generally used for shorter durations.
- Burst Mode: Some units offer a burst mode, where a series of high-frequency pulses are delivered in low-frequency bursts. This can be comfortable and may combine aspects of both mechanisms.
- Intensity (Amplitude): The intensity should be set to a level that produces a strong but comfortable tingling, buzzing, or tapping sensation. It should not be painful. For low-frequency TENS, the intensity should be just enough to cause a visible muscle twitch, but not a strong, uncomfortable contraction. Always start with a low intensity and gradually increase it.
Duration: The duration of TENS treatment for OA can vary based on individual response and the chronicity of the pain:
- Acute flare-ups: TENS can be used for 30-60 minutes, several times a day, as needed.
- Chronic OA pain: TENS can be used for longer durations, typically 30-90 minutes per session, up to 2-3 times a day. Some individuals with chronic pain may use TENS for several hours a day, taking short breaks (e.g., 10-15 minutes every 1-2 hours) to allow the skin to breathe and prevent irritation.
- The effects often last as long as the unit is on and for a period afterward. For chronic OA, consistent use is often recommended for sustained pain management.
Results
The effectiveness of TENS for osteoarthritis pain is a subject of ongoing research, with varying findings. Many individuals report experiencing significant pain relief during and immediately after TENS treatment. This can lead to:
- Reduced pain intensity: TENS can help decrease the perceived level of pain.
- Improved function: By reducing pain, TENS can facilitate better participation in physical therapy, exercise, and daily activities.
- Decreased medication reliance: Some individuals may find they need less pain medication when consistently using TENS.
- Enhanced quality of life: Overall, managing pain can contribute to a better quality of life.
However, TENS is generally considered a symptomatic treatment and does not alter the underlying progression of osteoarthritis. Its long-term efficacy can vary, and some studies suggest that the benefit may diminish over time for some individuals (tolerance development). The most benefit is often seen when TENS is used as part of a multimodal approach that includes exercise, weight management (if applicable), and other recommended therapies.
Side Effects and Precautions
TENS is generally considered a safe, non-invasive therapy with a low incidence of serious side effects. Most side effects are minor and reversible:
- Skin irritation: The most common side effect is localized skin irritation, redness, itching (pruritus), or a rash beneath the electrodes. This can be due to adhesive sensitivity, prolonged use, or infrequent electrode changes. Using hypoallergenic pads, rotating electrode placement, and ensuring clean, dry skin can help.
- Uncomfortable sensations: Some individuals may find the tingling, buzzing, or prickling sensation to be uncomfortable or unpleasant, especially if the intensity is too high.
- Allergic reaction: Rarely, an allergic reaction to the electrode gel or adhesive can occur.
- Burns: Although rare, electrical burns can occur if the intensity is set excessively high, if electrodes are faulty, or if there is poor skin contact. Always ensure the sensation is comfortable and strong, but never painful.
Contraindications and precautions:
It is crucial to consult a healthcare professional before using TENS, especially if you have any of the following conditions:
- Pacemaker or other implanted electrical devices: TENS can interfere with the function of these devices.
- Epilepsy: TENS may trigger seizures in susceptible individuals.
- Pregnancy: Avoid using TENS over the abdomen or lower back during pregnancy, unless specifically advised by a doctor or midwife.
- Heart conditions: Use with caution and under medical supervision, especially avoiding electrode placement across the chest.
- Cancer: Avoid placing electrodes over known or suspected malignant tumors.
- Numb, irritated, broken, or infected skin: Do not place electrodes on these areas.
- Driving or operating machinery: Do not use TENS while engaging in activities where a sudden muscle twitch or distraction could be dangerous.
- While sleeping or in the shower/bath: Avoid using TENS in these situations.
- Children: Use TENS on children only under strict medical supervision.
Conclusion
Transcutaneous Electrical Nerve Stimulation (TENS) offers a valuable, non-pharmacological option for managing the pain associated with osteoarthritis. By understanding its indications, precise electrode placement, dual mechanisms of action (gate control and endorphin release), and appropriate application parameters, individuals can effectively integrate TENS into their OA management strategy. While it provides symptomatic relief rather than a cure, TENS can significantly contribute to reducing pain, improving joint function, and enhancing the overall quality of life for those living with osteoarthritis. Always consult with a healthcare professional or physical therapist to determine if TENS is appropriate for your specific condition and to receive personalized guidance on its safe and effective use.
