Transcutaneous Electrical Nerve Stimulation (TENS): A Comprehensive Guide
Introduction: Pain is a complex and often debilitating experience that affects millions worldwide. While pharmacological interventions play a significant role in pain management, non-pharmacological approaches offer valuable alternatives and adjuncts. Among these, Transcutaneous Electrical Nerve Stimulation (TENS) stands out as a widely used and often effective modality. TENS involves the application of low-voltage electrical current through electrodes placed on the skin, aiming to alleviate pain by stimulating nerves. This article will delve into the intricacies of TENS, covering its indications, mechanism of action, practical application, anticipated results, and potential side effects.
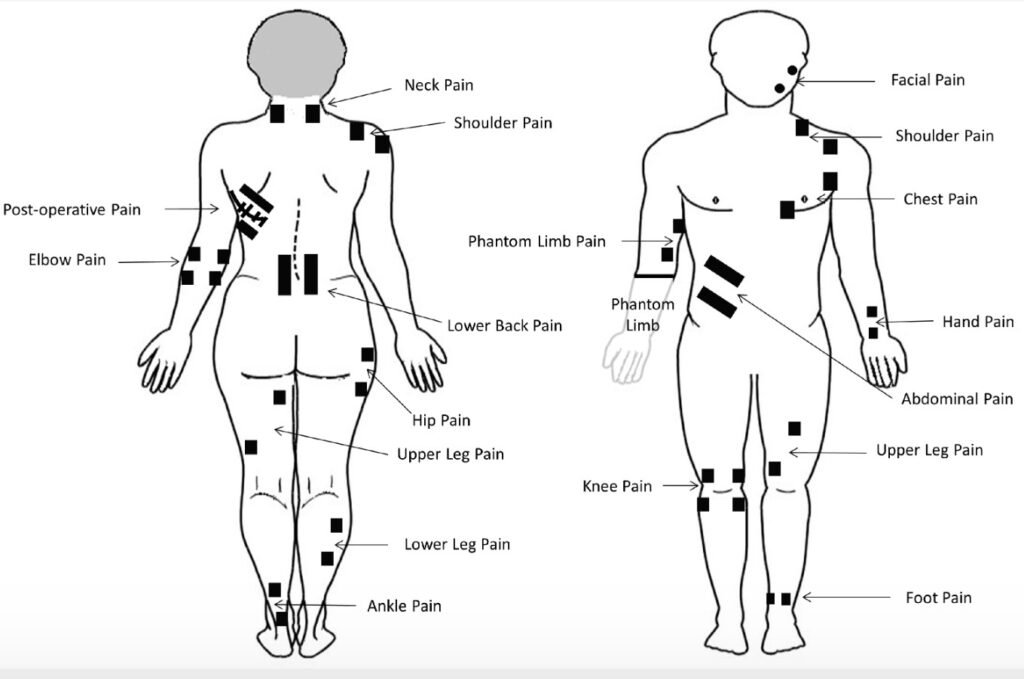
Indications: TENS is a versatile tool used for a wide range of acute and chronic pain conditions. Its non-invasive nature and relative safety make it a popular choice for both clinical and home use. Common indications for TENS include:
- Musculoskeletal Pain:
- Low back pain (acute and chronic)
- Neck pain
- Osteoarthritis (especially knee and hand)
- Rheumatoid arthritis
- Fibromyalgia
- Tendonitis
- Bursitis
- Myofascial pain syndrome
- Neuropathic Pain:
- Diabetic neuropathy
- Post-herpetic neuralgia
- Sciatica
- Phantom limb pain
- Complex regional pain syndrome (CRPS)
- Post-operative Pain:
- To reduce reliance on opioid analgesics and improve recovery.
- Obstetric Pain:
- Labor pain management.
- Other Pain Conditions:
- Dysmenorrhea (menstrual pain)
- Headaches (tension-type and migraine)
- Trigeminal neuralgia
It’s important to note that TENS is generally more effective for localized pain rather than widespread, diffuse pain, though it can be used as an adjunct in conditions like fibromyalgia.
Mechanism of Action: The precise mechanisms by which TENS alleviates pain are multifaceted and thought to involve several neurophysiological pathways. The two primary theories are:
- Gate Control Theory of Pain (Melzack and Wall, 1965): This is the most widely accepted theory. According to this theory, the substantia gelatinosa in the spinal cord acts as a “gate” that can either block or allow pain signals to pass to the brain. TENS, by stimulating large diameter, non-nociceptive (non-pain transmitting) afferent nerve fibres (A-beta fibres), activates inhibitory interneurons in the spinal cord. This activation effectively “closes the gate,” inhibiting the transmission of pain signals carried by smaller diameter nociceptive fibers (A-delta and C fibers) from reaching the brain. The sensation of TENS (a tingling or buzzing) overrides the pain sensation, essentially distracting the nervous system.
- Opioid Release Theory: High-frequency TENS (>50 Hz) and low-frequency TENS (<10 Hz) are believed to stimulate the release of endogenous opioids (e.g., endorphins, enkephalins, dynorphins) from various brain regions, including the periaqueductal gray matter and raphe nuclei. These opioids act as natural painkillers, binding to opioid receptors and modulating pain perception at both spinal and supraspinal levels. Low-frequency TENS is particularly associated with endorphin release, while high-frequency TENS may primarily involve enkephalins.
Additionally, TENS may contribute to pain relief through other mechanisms, including:
- Improved blood circulation: By causing vasodilation in the treated area.
- Muscle relaxation: By reducing muscle spasms and tension.
- Reduction of edema: By promoting fluid movement.
- Placebo effect: As with any treatment, the patient’s belief in the therapy can contribute to pain reduction.
Location of Electrodes
Correct electrode placement is crucial for effective TENS therapy. The general principles for electrode placement include:
- Around or Directly Over the Painful Area: This is often the most straightforward approach. Electrodes are placed on either side of or directly on the painful site.
- Along the Dermatome: If the pain follows a specific nerve distribution, electrodes can be placed along the corresponding dermatome (area of skin supplied by a single spinal nerve).
- Over Nerve Pathways: Placing electrodes over the main nerve trunk innervating the painful area can be effective.
- Acupuncture Points or Trigger Points: Some practitioners find success by placing electrodes on known acupuncture points or myofascial trigger points associated with the pain.
- Contralateral Side: In some cases, for example, for phantom limb pain, electrodes may be placed on the corresponding area of the unaffected limb.
General Guidelines:
- Clean Skin: Ensure the skin is clean, dry, and free of lotions or oils to ensure good adhesion and conductivity.
- Electrode Spacing: Electrodes should be placed at least 1 inch apart to allow for proper current flow. Closer spacing tends to concentrate the current, while wider spacing spreads it out.
- Avoid Bony Prominences: Do not place electrodes directly over bony prominences, as this can be uncomfortable and less effective.
- Avoid Anterior Neck and Eyes: Never place electrodes on the anterior neck (carotid sinus) due to the risk of affecting heart rate or blood pressure, or near the eyes.
- Avoid Areas of Impaired Sensation: If sensation is significantly impaired, the patient may not be able to adequately report discomfort, leading to potential skin irritation.

Frequency, Duration, and Intensity
These parameters are crucial for optimizing TENS treatment and are often adjusted based on the individual’s pain, the type of TENS desired, and the desired physiological effect.
- Frequency (Pulse Rate): Measured in Hertz (Hz) or pulses per second (pps).
- High Frequency (Conventional TENS): Typically, 80−150 Hz. This setting is thought to primarily activate the gate control mechanism, providing rapid, but often short-lived, pain relief. The sensation is usually a comfortable, buzzing or tingling.
- Low Frequency (Acupuncture-like TENS – ALTENS): Typically, 1−10 Hz. This setting is associated with the release of endogenous opioids, providing longer-lasting pain relief but often requiring a higher intensity that produces a muscle twitch.
- Burst Mode: A variation of low-frequency TENS where pulses are delivered in short bursts. This also aims to stimulate opioid release and can be more comfortable for some individuals than continuous low-frequency stimulation.
- Pulse Width (Pulse Duration): Measured in microseconds ($\mu$s). This refers to the duration of each electrical pulse.
- Generally, a pulse width between $50-250 \mu$s is used. Wider pulse widths deliver more energy and can recruit more nerve fibres.
- Intensity (Amplitude): Measured in milliamperes (mA). This refers to the strength of the electrical current.
- The intensity should be adjusted to a level that the patient finds comfortable but effective.
- For conventional TENS, the goal is a strong, comfortable tingling sensation without muscle contraction.
- For low-frequency TENS, a visible muscle twitch is often desired to maximize opioid release, but this should still be tolerable for the patient.
- Duration of Treatment:
- TENS can be applied for varying durations, from 20-30 minutes for acute pain episodes to several hours intermittently throughout the day for chronic pain.
- For chronic conditions, patients may wear the unit for extended periods, turning it on as needed for pain relief.
- It’s important to monitor skin integrity, especially with prolonged use.
Results and Efficacy
The effectiveness of TENS varies widely among individuals and pain conditions. While some people experience significant pain relief, others may find it less beneficial.
Positive Results:
- Reduced Pain Intensity: Many users report a decrease in their subjective pain levels.
- Decreased Reliance on Analgesics: TENS can help reduce the need for pain medication, particularly opioids, which can have significant side effects.
- Improved Function: By reducing pain, TENS can facilitate increased activity, mobility, and participation in daily activities and rehabilitation exercises.
- Better Sleep: Less pain often leads to improved sleep quality.
- Enhanced Quality of Life: Overall, effective pain management contributes to a better quality of life.
Factors Influencing Results:
- Type of Pain: TENS tends to be more effective for localized, neuropathic, and musculoskeletal pain.
- Individual Variability: Response to TENS is highly individual.
- Correct Application: Proper electrode placement, frequency, duration, and intensity are critical.
- Patient Compliance: Consistent and correct use of the device.
- Underlying Condition: TENS treats the symptom (pain) and not the underlying cause of the pain. It’s often part of a broader pain management plan.
While numerous studies support the efficacy of TENS for various pain conditions, the level of evidence can vary. Some studies show strong support, while others suggest more moderate benefits. Meta-analyses and systematic reviews generally conclude that TENS can be an effective adjunct in pain management, particularly for chronic musculoskeletal pain.
Side Effects and Contraindications
TENS is generally considered safe with few significant side effects when used correctly.
Common Side Effects (usually mild):
- Skin Irritation: Redness, itching, or rash under the electrodes. This can often be minimized by using hypoallergenic electrodes, rotating electrode placement, and ensuring clean skin.
- Discomfort or Burning Sensation: If the intensity is too high or electrodes are not making good contact.
- Allergic Reaction: To the electrode gel or adhesive.
Contraindications (when TENS should NOT be used):
- Cardiac Pacemakers or Implanted Defibrillators: Electrical currents can interfere with the function of these devices.
- Pregnancy (over the abdomen/pelvis): While TENS is sometimes used for labour pain, it is generally contraindicated over the abdomen and pelvis during early pregnancy due to theoretical risks to the foetus. Consultation with a healthcare professional is essential.
- Epilepsy (over the head/neck): Can potentially induce seizures.
- Areas of Impaired Sensation: Increased risk of skin damage due to inability to perceive discomfort.
- Over the Eyes or Anterior Neck (carotid sinus): As mentioned earlier, due to risks to vision and cardiovascular function.
- Over Malignancy: There is a theoretical concern that electrical stimulation could promote the spread of cancer cells, though this is not definitively proven.
- Deep Vein Thrombosis (DVT) or Thrombophlebitis: To avoid dislodging a clot.
- Active Bleeding or Haemorrhage: Can exacerbate bleeding.
Precautions (use with caution and under professional guidance):
- Individuals with heart disease (other than pacemakers).
- Over damaged or broken skin.
- In children (use with extreme caution and professional supervision).
- Cognitively impaired individuals.
Conclusion
Transcutaneous Electrical Nerve Stimulation (TENS) offers a valuable, non-pharmacological option for managing a diverse range of acute and chronic pain conditions. Its ease of use, portability, and relatively low risk profile make it an attractive choice for both clinical and home settings. While not a cure for underlying conditions, TENS can significantly contribute to pain relief, reduce reliance on medications, and improve functional outcomes and quality of life for many individuals. Understanding its mechanisms, proper application techniques, and potential contraindications is paramount for maximizing its benefits and ensuring safe use. As with any medical intervention, consultation with a healthcare professional is always recommended before initiating TENS therapy.
